Association between cardiometabolic index and risk of testosterone deficiency in adult men: a cross-sectional study | BMC Public Health

Study design and participants
The NHANES is a publicly accessible program designed to assess the health and nutritional status of individuals across all age groups in the United States. It is overseen and conducted by the National Center for Health Statistics (NCHS) at the US Centers for Disease Control and Prevention (CDC). The survey is carried out biennially, enrolling approximately 5,000 individuals from various counties nationwide. The collected data are made available to researchers globally and include demographic, dietary, physical examination, laboratory, and questionnaire data. The sample collection employs a complex, multistage, probability sampling design to ensure unbiased estimates of the national population. More information about NHANES methods and protocols can be found on their official website. All study designs and protocols of NHANES were approved by the NCHS Research Ethics Review Board, and conducted in accordance with the Declaration of Helsinki. All participants provided written informed consent prior to participation.
Initially, a total of 29,902 participants were included from three NHANES cycles: 2011–2012, 2013–2014, and 2015–2016. Figure 1 illustrates the detailed sample selection process. Specific exclusion criteria were applied as follows: (1) Female participants (n = 15,151), (2) Participants under the age of 20 (n = 6,506), (3) Participants without testosterone data or CMI-related information (n = 4,158), (4) Participants without data on potential covariates (n = 1,340). After excluding participants who met the above criteria, a total of 2,747 participants were retained and included in the final statistical analysis.
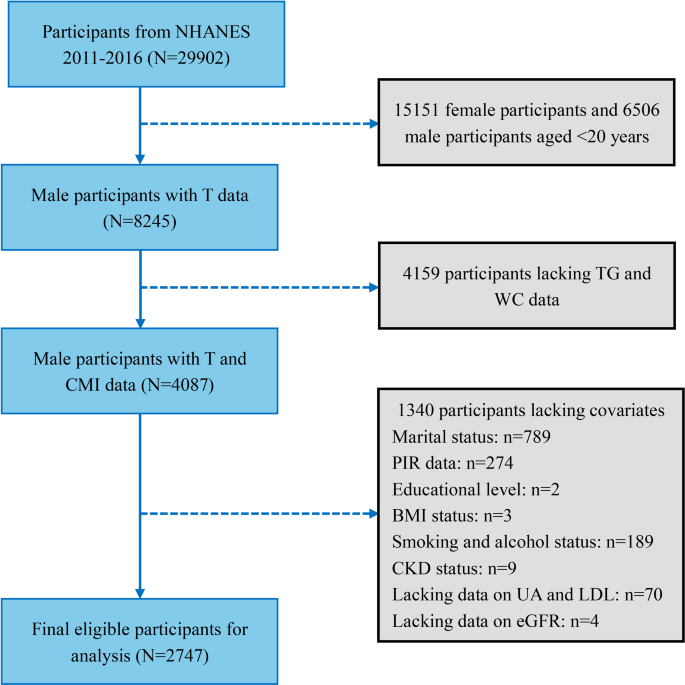
Flowchart of participant selection and exclusion criteria. NHANES, National Health and Nutrition Examination Survey; T, Testosterone; TG, Triglycerides; WC, Waist Circumference; PIR, Poverty Income Ratio; BMI, Body Mass Index; CKD, Chronic Kidney Disease; UA, Uric Acid; LDL, Low-Density Lipoprotein; eGFR, Estimated Glomerular Filtration Rate
Calculation of the CMI
According to the formula, the CMI is calculated by combining blood biochemical indices and body measurement indices, including triglycerides (TG), HDL-c, waist circumference (WC), and height [16]. The calculation formula is:
CMI=(TG/HDL-c) × (WC/Height).
Blood sample collection and processing were conducted by trained technicians at the Mobile Examination Center (MEC) following standardized sample handling procedures. The biochemical measurements included total cholesterol (TC), TG, HDL-c, low-density lipoprotein cholesterol (LDL-C), uric acid (UA), and estimated glomerular filtration rate (eGFR). All participants were required to fast for more than 8 h before blood collection. Body measurements were also completed at the MEC, including height, weight, and WC.
Definition of the outcomes
Serum total testosterone (TT) and the clinically defined testosterone deficiency (TD) were our two primary outcomes. To account for the diurnal variation in hormone secretion, we selected only adult men who completed their laboratory examinations in the morning, ensuring a more representative measurement of TT levels. Testosterone measurements were performed using isotope dilution high-performance liquid chromatography tandem mass spectrometry (ID-LC-MS/MS), a method capable of high-throughput processing of large sample volumes with a detection limit of 0.75 ng/dL. According to the guidelines of the American Urological Association (AUA), the diagnosis of TD is based on a combination of TT levels < 300 ng/dL and corresponding clinical symptoms [21]. Due to database limitations and the inability to access participants’ clinical symptoms, we cautiously used TT < 300 ng/dL as the criterion for diagnosing TD, consistent with previous related studies [15, 22,23,24].
Assessments of covariates
Potential covariates were selected based on previous literature and included factors that might influence the relationship between testosterone and CMI. These covariates included demographics, biochemical indices, lifestyle habits, and medical comorbidities. Demographic characteristics included age (categorized into 20-40y, 40-60y, and > 60y), BMI (categorized into < 25 kg/m2, 25–30 kg/m2, and > 30 kg/m2), family income (measured by the Poverty Income Ratio (PIR) and categorized into < 1.3, 1.3–3.5, and > 3.5), race (Non-Hispanic White, Non-Hispanic Black, Mexican American, Other Race, and Other Hispanic), education level (less than high school, high school graduate, and more than high school), and marital status (categorized as Solitude and Cohabitation). Biochemical indices included LDL-c, TG, UA, and eGFR.
Lifestyle habits included alcohol consumption and smoking. Alcohol consumption was defined based on whether the average annual intake exceeded 12 drinks, classifying participants as drinkers or non-drinkers. Smoking status was determined based on whether participants had smoked more than 100 cigarettes in their lifetime and whether they currently smoked. Participants were classified as current smokers if both conditions were met, non-smokers if neither condition was met, and former smokers otherwise. Medical comorbidities included hypertension, diabetes, hyperlipidemia, cardiovascular disease (CVD), and chronic kidney disease (CKD). Hypertension was defined as having a previous diagnosis, taking antihypertensive medication, or having a measured blood pressure ≥ 140/90 mmHg. Diabetes was defined as having a previous diagnosis, taking antidiabetic medication, hemoglobin A1c level ≥ 6.5%, fasting plasma glucose level ≥ 126 mg/dL, or a plasma glucose level ≥ 200 mg/dL at 2 h after an oral glucose tolerance test (OGTT). Prediabetes was diagnosed according to the criteria set by the American Diabetes Association. Specifically, prediabetes was defined as having one of the following: (1) FPG levels between 100 and 125 mg/dL, (2) a 2-hour plasma glucose level between 140 and 199 mg/dL after OGTT, or (3) Hemoglobin A1c levels between 5.7% and 6.4%. Hyperlipidemia was defined as having TC ≥ 5.17 mmol/L, LDL-c ≥ 3.36 mmol/L, HDL-c < 1.03 mmol/L, or TG ≥ 1.69 mmol/L. CVD was defined based on a history of congestive heart failure, coronary heart disease, angina, or heart attack. CKD was defined as having an eGFR < 60 ml/min per 1.73 m² according to the CKD Epidemiology Collaboration creatinine equation, equivalent to CKD stages 3–4 [25].
Statistical analysis
Based on the complex sampling design of NHANES, all statistical analyses applied appropriate sample weights to each participant to ensure the representativeness of the statistical results. When describing the basic characteristics of the sample, continuous variables were presented as weighted means ± standard errors (SE), while categorical variables were expressed as weighted percentages. For group comparisons, weighted linear regression was used for continuous variables and weighted chi-square tests for categorical variables. Linear regression analysis and logistic regression analysis were employed for different outcomes. The results of the linear regression analysis were expressed as beta coefficients and 95% confidence intervals (CIs), while the results of the logistic regression analysis were expressed as odds ratios (ORs) and 95% CIs. To improve the stability and reliability of our results, we used different models to adjust for potential covariates in both types of regression analyses. Model 1 included only the exposure variable. Model 2 adjusted for age, race, marital status, education, PIR, and BMI. Model 3 further adjusted for all remaining potential covariates, including UA, TC, LDL, eGFR, lifestyle habits, and medical comorbidities. During the analysis, CMI was further converted into quartile variables for analysis, with Q1 as the reference. We also conducted trend tests for the quartile variables of CMI using linear regression analysis.
To test the stability of the statistical results across different population characteristics, we conducted subgroup analyses and interaction tests for key demographic and health-related factors, including age, BMI, smoking status, DM, hypertension, CVD, and CKD. To investigate whether CMI is linearly related to TT or the risk of TD, we used smooth curve fitting and generalized additive models. Finally, ROC curve analysis was employed to compare the predictive diagnostic value of CMI for TD, expressed as the area under the curve (AUC) and 95% CI. All statistical analyses were conducted using EmpowerStats ( X&Y Solutions, Inc.) and the statistical software packages R ( The R Foundation). Statistical significance was defined as a two-sided p-value of less than 0.05.
link




:max_bytes(150000):strip_icc()/Foods-to-Prioritize-in-January-for-Heart-Health-a9e789765ec849b99d8f71497b797700.jpg)