Nirsevimab Greatly Reduced Severe RSV in Infants
For infants in their first RSV season, the monoclonal antibody Nirsevimab (Beyfortus) was 80% effective against RSV-related ICU admission and 83% effective against acute respiratory failure.
RT’s Three Key Takeaways:
- High Effectiveness: Nirsevimab was shown to be highly effective—80% against RSV-related ICU admission and 83% against acute respiratory failure—in infants during their first RSV season.
- Strong Real-World Evidence: Data from a large, multicenter US network demonstrated consistent protection across diverse infants, most of whom were previously healthy.
- Public Health Support: These findings reinforce CDC recommendations to use monoclonal antibodies (nirsevimab or clesrovimab) or maternal vaccination to prevent severe RSV outcomes in infants.
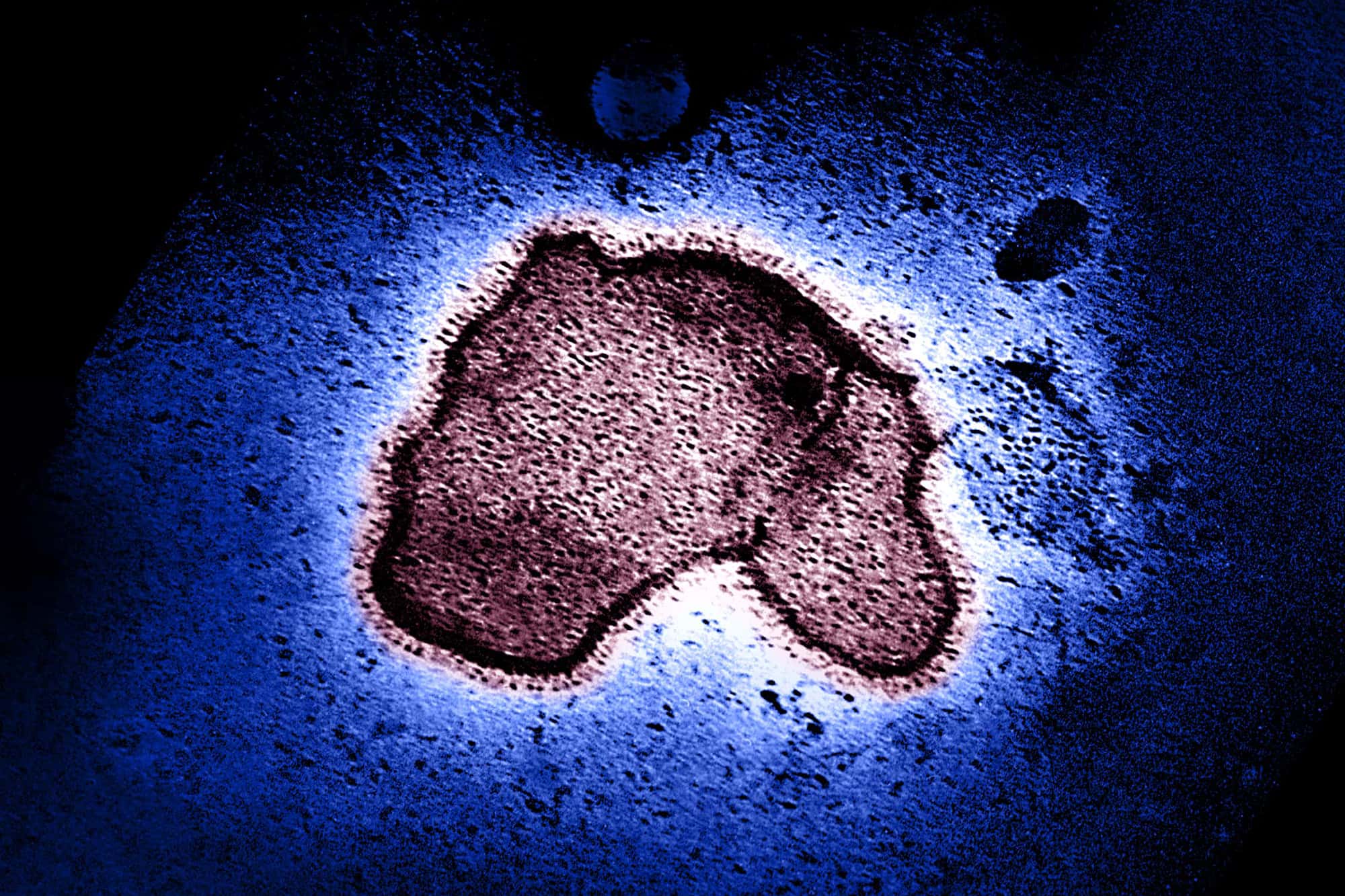
Respiratory syncytial virus (RSV) remains a leading cause of ICU admission and respiratory failure among infants in the United States, particularly for those in their first year of life. In August 2023, the CDC’s Advisory Committee on Immunization Practices (ACIP) recommended nirsevimab (Beyfortus), a long-acting monoclonal antibody, for all infants younger than 8 months entering their first RSV season, unless protected through maternal RSV vaccination. Although early post-licensure data showed strong protection against RSV-related hospitalization, evidence regarding prevention of critical illness had been limited. A new investigation, conducted across 27 hospitals in 24 states during the 2024–25 RSV season, provides the clearest real-world assessment to date of nirsevimab’s ability to prevent the most severe RSV outcomes.
The study used a case-control design within the CDC-funded Overcoming RSV Network, enrolling infants under 1 year of age admitted to an ICU with respiratory symptoms. Case-patients were those with laboratory-confirmed RSV infection; control patients tested negative for RSV but had similar respiratory illness requiring ICU care. Infants were included only if their symptoms began within 14 days before hospitalization and if their RSV immunization status could be verified. Nirsevimab receipt was counted only when given at least seven days before symptom onset.
After exclusions, the analysis included 457 RSV-positive case-patients and 302 RSV-negative controls. The two groups were similar in terms of demographic characteristics and geographic distribution, though underlying medical conditions were more common among controls. Among the RSV-positive infants, 14% had received nirsevimab at least a week before symptoms, compared with 45% of RSV-negative controls.
The investigation assessed two major outcomes: RSV-associated ICU admission and acute respiratory failure, defined as the need for advanced respiratory support beyond a child’s baseline level, including continuous positive airway pressure (CPAP), bilevel positive airway pressure (BiPAP), or invasive mechanical ventilation. More than half of infants in both groups met criteria for acute respiratory failure.
The findings showed that nirsevimab provided substantial protection. The monoclonal antibody was 80% effective against RSV-related ICU admission and 83% effective against acute respiratory failure. For both outcomes, infants had typically received their dose about 50–52 days before symptom onset. When effectiveness was examined by time since receipt, protection remained strong: 86% effectiveness in the first 7–59 days after administration and 66% effectiveness from 60 to 183 days. A secondary analysis that considered only matched case-control pairs yielded similar results, demonstrating 76% effectiveness against ICU admission.
This large multi-site investigation has several strengths, including its broad geographic scope and systematic verification of immunization records. Previous post-licensure evaluations of nirsevimab’s performance were limited to single-health-system studies or international data. The present findings closely align with pooled international estimates, reinforcing the conclusion that nirsevimab is highly effective in preventing severe RSV disease. The study also found that most infants admitted to an ICU with RSV were previously healthy and born at term—consistent with longstanding observations that severe RSV can affect otherwise low-risk infants.
The authors note several limitations. Clinical RSV testing protocols varied across hospitals, raising the possibility that co-infections were not fully assessed. Maternal RSV vaccination status might also have been incompletely captured. In addition, the study could not precisely measure the duration of protection, although the results suggest meaningful defense extending several months. As with all observational studies, residual confounding cannot be ruled out.
Despite these limitations, the evidence strongly supports ACIP recommendations that infants be protected against RSV through either maternal vaccination or monoclonal antibody administration. With the June 2025 addition of clesrovimab as another infant monoclonal antibody option, clinicians now have multiple tools to safeguard infants during their first RSV season. This new analysis demonstrates that nirsevimab meaningfully reduces the risk of the most dangerous RSV outcomes—ICU admission and respiratory failure—and can help guide discussions between healthcare providers and families seeking effective RSV prevention strategies.
link