Maternal glucose homeostasis during pregnancy in women with overweight or obesity and offspring metabolic health

Study design
This paper includes data from the APPROACH (An Optimized Programming of Healthy Children) study, which was a randomized controlled trial (RCT) conducted at Copenhagen University Hospital Herlev-Gentofte and the University of Copenhagen, Department of Nutrition, Exercise, and Sports (Copenhagen, Denmark). The RCT included a dietary intervention in women during pregnancy and was conducted from January 2014 to December 2017. This was followed by a longitudinal cohort study of the offspring born to participating women. Data on the offspring was collected at birth, 3 and 5 years of age, and collected from June 2014 to January 2023. A detailed description of the APPROACH study design and methodology can be found elsewhere18. The study was approved by the Ethical Committee of the Capital Region of Denmark (H-3–2013-119) and was registered at ClinicalTrials.gov (NCT01894139). All study procedures were conducted in accordance with the Helsinki II Declaration.
Participants
Pregnant women received information about the study during their trans-nuchal scan (from 11 weeks and 4 days to 13 weeks and 6 days of gestation). Women were eligible for inclusion if they had a singleton pregnancy, had a pre-pregnancy BMI between 28–45 kg/m2, and were older than 18 years. The women and their partner received both written and oral information about the study before signing an informed consent. Women were excluded if they developed GDM, defined in Denmark as a 2-h OGTT glucose concentration ≥ 9.0 mmol/L13, at any time point during the study.
Intervention
Included women were allocated in groups of 4–8 and subsequently randomized in a 1:1 ratio to one of two diets: i) the intervention diet characterized by high protein content (25% of total energy intake) and a low glycemic index of ~ 45, or ii) the control diet, with moderate protein content (18% of total energy intake) and a moderate glycemic index of ~ 54, aligning with the Nordic Nutritional Recommendations from 201219. Fat provided ~ 30% of calories in both diets. The women received nutrition guidance from a clinical dietician and were instructed to consume the diets ad libitum18.
Maternal anthropometry
At the baseline visit (GW 15), height was measured to the nearest 0.5 cm by a wall-mounted stadiometer (Seca, Germany), and body weight was measured to the nearest 0.1 kg by a medical scale (Tanita, Illinois, USA). Body weight was subsequently measured prior to every counseling session with the clinical dietitian (up to nine times during pregnancy). Accumulated GWG in GW 15, 28, and 36 was calculated as measured body weight at these time points minus pre-pregnancy body weight. Pre-pregnancy weight was self-reported or obtained by the general practitioner in GW 6–8. These values correlated with measured weight at GW 15 (R2 = 0.94). BMI was calculated as weight (kg) divided by height squared (m2). Parity was obtained by questionnaires and categorized as 0, 1, or ≥ 2.
Offspring anthropometry
At birth, midwives at the Copenhagen University Hospital Herlev-Gentofte obtained anthropometric measurements from the offspring. At 3 years (± 4 weeks) and 5 years (± 4 weeks) of age, anthropometric measurements were obtained by trained staff at the University of Copenhagen, Department of Nutrition, Exercise, and Sports, Copenhagen, Denmark.
At birth, the length was measured by using a non-elastic measuring tape to the nearest 0.5 cm. At 3 and 5 years of age, height was measured by using a wall-mounted stadiometer to the nearest 0.5 cm (Seca, Germany). Body weight at birth was measured by a medical beam scale (Tanita, USA) to the nearest 10 g and at 3, and 5 years of age, body weight was measured by a bioelectrical impedance scale (InBody570, USA) to the nearest 100 g.
Z-scores were calculated according to the WHO 2006 standards20 using the WHO Anthro software21 which includes children up to 60 months (5 years) of age. The WHO 2007 Reference for School-age Children and Adolescents (5 to 19 years) was used to calculate z-scores in children aged 61 months22.
Maternal blood markers
In GW 15, 28, and 36, venous blood samples from the women were drawn after an overnight fast (≥ 10 h) at the Copenhagen University Hospital Herlev-Gentofte. Samples were analyzed for fasting plasma glucose, glycated hemoglobin (HbA1c), C-peptide, total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, very-low lipoprotein (VLDL) cholesterol, and triglycerides (TG). Moreover, the participants performed a 2-h 75-g OGTT in GW 28.
Offspring blood markers
Umbilical cord blood was collected at birth, and venous blood samples were collected at 3 years of age (after a 2-h fast) and at 5 years of age (after an overnight fast of ≥ 8 h). Samples were analyzed for fasting glucose, insulin, C-peptide, insulin growth factor-1 (IGF-1), insulin growth factor binding protein-3 (IGFBP-3), C-reactive protein (CRP), total cholesterol, LDL-cholesterol, HDL-cholesterol, and TG. All analyses were measured in plasma, except for glucose which was analyzed in whole blood.
Glucose at birth was measured using a colorimetric method, on a Pentra 400 analyzer (Horiba ABX). Fasting glucose at 3 and 5 years was analyzed on the same day as the blood sampling with Hemocue Glucose 201+ (HemoCue, Danmark).
Insulin, C-peptide, IGF-1, and IGFBP-3 were analyzed on Immulite 2000 (Siemens Healthcare, UK) and total cholesterol, LDL-cholesterol, HDL-cholesterol, TG, and CRP were analyzed on Pentra 400 (Horiba ABX SAS, France). For insulin concentration below 14.4 pmol/L (limit of detection), serum was used and analyzed with an ultrahigh sensitive insulin ELISA kit from Mercodia AB (cat no. 10–1132-01).
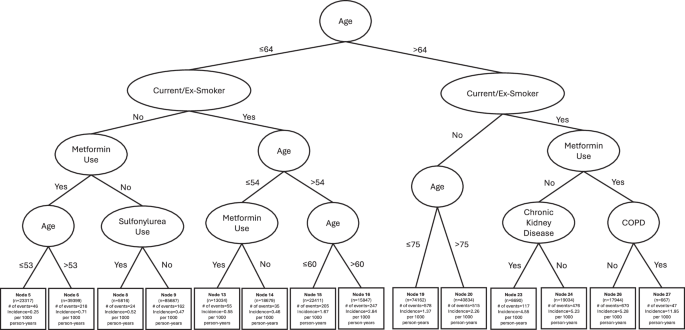
Statistical analysis
In this secondary analysis, the two diet arms of the primary RCT were pooled because there was no effect of the dietary intervention on maternal blood metabolic biomarkers18. To eliminate potential overlooked effects of the intervention, we adjusted for the allocated diet intervention group.
Histograms were used to visually evaluate data distributions. Characteristics of pregnant women and offspring are presented as mean ± standard deviation (SD) for normally distributed variables and as median with quartiles (Q1;Q3) for skewed variables. Categorical variables are presented as absolute and relative frequencies.
Available case analysis was carried out using a linear mixed model that included time as a fixed factor and subject ID as a random effect to examine the association of maternal fasting glucose concentrations in GW 15, GW 28, GW 36, and 2-h OGTT glucose concentration in GW 28 with offspring metabolic biomarkers and BMI z-score from birth to 5 years of age. A simple linear regression model was utilized to examine the association of maternal glycemia and weight-for-length at birth. We evaluated the models for normal distribution using qq-plots and residual plots to check for heteroscedasticity and linearity. If the model did not fulfill the model assumptions, outcomes were log-transformed, and β-estimates and 95% confidence intervals (CI) were back-transformed and are expressed as percentage changes. Otherwise, data is reported as β-estimates with 95% CI and corresponding p-values. The analyses were adjusted for potential confounders, with Model 1 being crude (unadjusted) and Model 2 being adjusted for pre-pregnancy BMI, allocated diet intervention group, accumulated gestational weight gain, gestational age, maternal age, parity, and offspring sex. A p-value < 0.05 was used to determine statistical significance. All statistical analyses were performed using R studio (version 4.2.2).
link